
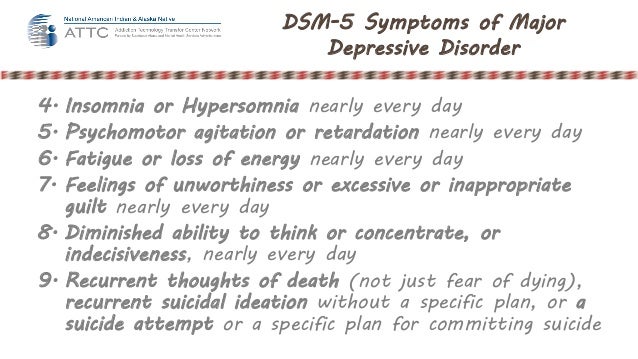

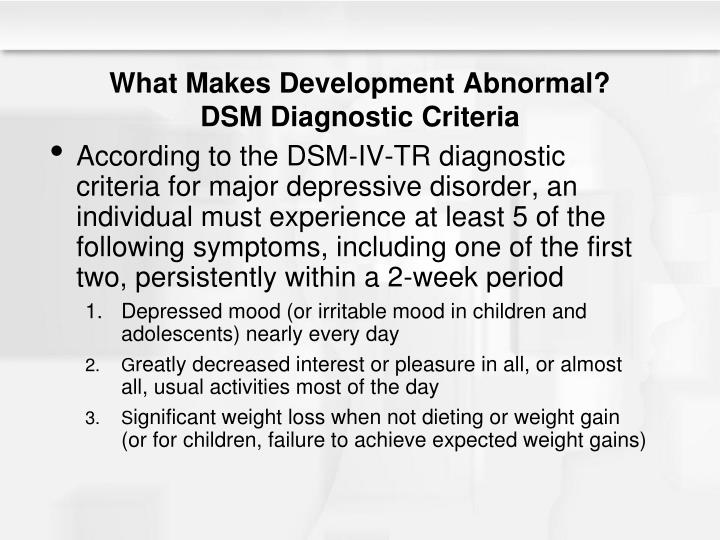
2012), we can estimate that DSM-5 bipolar II disorder will be diagnosed about twice as often as heretofore and have a prevalence approaching that of bipolar I.Ī more frequent diagnosis of bipolar II disorder is both justified and logical: a milder condition (in this case hypomania) is usually more prevalent than a severe one (mania). On the basis of the Bridge Study data (Angst et al. In addition, DSM-5 provides new formal criteria for substance/medication-induced bipolar and related disorder. DSM-5, like DSM-IV, allows some scope for clinical judgment as to causality. In DSM-5, that change - provided it persists at fully syndromal level beyond the physiological effect of the treatment - is explicitly a criterion for bipolar II disorder. In DSM-IV, the change of major depression into hypomania under antidepressant treatments (ADs) was in principle an exclusion criterion. One important and amply justified change in DSM-5 concerns the diagnosis of bipolar II disorder. As the international Bridge Study of 5,635 patients seeking treatment for major depressive episodes demonstrated clearly, any of those three gate questions is valid on its own, according to the criteria established by Robins and Guze ( 1970) and Angst et al. This strict new rule is not based on data, indeed it contradicts available evidence. Thus, for no apparent reason, DSM-5 classifies some patients as having subthreshold bipolar disorders who would formerly have been diagnosed with manic episodes or bipolar I or II disorders. This new rule is, of course, more restrictive and excludes all individuals who report only one of the three entry symptoms and those with both elated and irritable mood. Where DSM-IV required, as criterion A, the presence of one of the two mood symptoms (elation/euphoric or irritable mood), in DSM-5, ‘the mood change must be accompanied by persistently increased activity or energy levels’. The main changes are three: (1) a problematic change concerning the gate questions (criterion A), (2) a welcome reduction in the number of exclusion criteria and (3) a vigorous effort to operationalize bipolar subthreshold syndromes, hitherto unified under the NOS heading. The definitions of both manic and hypomanic episodes have been radically revised, which will impact on both bipolar diagnoses. However, it is now possible to specify both depressive disorders and bipolar disorders with mixed features. The main lines of the DSM-5 definition of major depressive episodes (MDE), basic to the diagnoses of both bipolar I and bipolar II disorders, are similar to those of DSM-IV: presence of five of nine diagnostic symptoms with a minimum duration of 2 weeks and a change from previous functioning. DSM-5 may also have an impact on patient selection for placebo-controlled drug trials with antidepressants. Nonetheless, overall, DSM-5 is a step in the right direction, specifying more subdiagnostic categories with an improved dimensional approach to severity. This restriction will unfortunately change the diagnoses of some patients from DSM-IV bipolar I and II disorders to subdiagnostic bipolar syndromes. The diagnosis of bipolarity now requires, as entry criterion A, not only the presence of elated or irritable mood but also the association of these symptoms with increased energy/activity.
In addition, hypomanic and manic episodes occurring during antidepressant treatments are, under certain conditions, accepted as criteria for bipolar disorders.

Several new subthreshold groups of depression, bipolar disorders and mixed states are now operationally defined in DSM-5.
#DSM 5 MAJOR DEPRESSIVE DISORDER MANUAL#
The diagnostic classification of mood disorders by the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) had two major shortcomings: an underdiagnosis of bipolar disorders and a large proportion of treated patients had to be allocated to the vague NOS groups ‘not otherwise specified’.


 0 kommentar(er)
0 kommentar(er)
